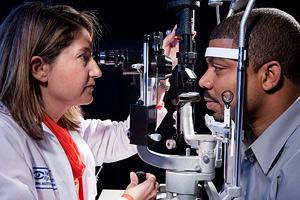
Eye Examination
People with type 1 diabetes who intensively control their blood glucose (blood sugar) early in their disease, versus those who do not, are 48 percent less likely to need eye surgery, and the total number of such surgeries is 37 percent less.
These reductions lead to ocular surgery costs about 32 percent lower for people who practice early tight glucose control. The findings are the latest results of the Diabetes Control and Complications Trial (DCCT) and its follow-up, the Epidemiology of Diabetes Control and Complications (EDIC) study. Results were published April 30 in the New England Journal of Medicine.
Eye diseases are a common complication for people with diabetes. More than 4 million Americans have diabetic retinopathy – damage to the small blood vessels in the retina – one of the leading causes of vision loss worldwide. People with diabetes are also at increased risk of developing cataracts and glaucoma.
“By controlling blood glucose early in the course of type 1 diabetes, people are less likely to have severe eye problems and to suffer vision loss,” said Dr. Catherine Cowie, director of programs in diabetes epidemiology within the NIH’s National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). “As results from the DCCT and EDIC studies show again and again, tight control of blood glucose early on for people with type 1 has far-reaching benefits for preventing or delaying many of the complications of diabetes.”
Beginning in 1983, the DCCT/EDIC study enrolled 1,441 people in the United States and Canada between ages 13 and 39 with recent-onset type 1 diabetes. In the DCCT, half were assigned at random to intensive blood glucose control designed to keep blood glucose as close to normal as safely possible, and half to the conventional treatment at the time.
The DCCT ended in 1993 when the intensive group was found to have substantially less eye, nerve and kidney disease. All participants were then taught intensive blood glucose control and followed during the ongoing EDIC study. The intensive group practiced tight blood glucose control an average 6.5 years longer than the control group. Average blood glucose has been similar in both groups since about five years after DCCT ended. In 2015, researchers reported that this early intensive blood glucose control lengthened life for people with type 1 diabetes.
In the current publication, after an average 23 years of follow-up, 130 ocular surgeries were performed on 63 people in the intensive group – 8.9 percent of that group. In the conventional treatment group, 189 ocular surgeries were performed on 98 people – 13.4 percent of that group.
Higher average blood glucose accounted for the increased long-term risk of ocular surgery in the conventional group. Most of the increased need for ocular surgery was associated with retinopathy severity. Other factors associated with ocular surgery included progression of diabetes-related kidney disease, nerve damage and high blood pressure.
This articled originally posted by and used with permission from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).