
Ellen Mazel, M. Ed., oversees the CVI assessment program at Perkins, where she estimates that 60% of the entire student body has CVI. Credit: Burju Sari
Nearly two decades ago, Ellen Mazel, M.Ed., a teacher for children with visual impairment at Perkins School for the Blind noticed a shift in her ability to meet her students’ needs.
"Increasingly, my usual teaching methods were not working for many of my students,” she said.
In hindsight it’s clear that her teaching methods, which were geared toward people with ocular causes of vision loss, were not as effective for a growing group of students with low vision due to cerebral (cortical) visual impairment (CVI). CVI is a condition that interferes with the ability of the brain to process information from the eyes.
A person with CVI has difficulty with visual processing – turning light from their eyes into meaningful information about the complex visual world around them. CVI can co-occur with ocular impairment, but the visual deficits cannot be explained by the eye condition alone because the functional vision deficits are predominately brain-based.
Today, Mazel oversees the CVI assessment program at Perkins, where she estimates that 60% of the entire student body has CVI.
Hiding in plain sight
Mounting evidence suggests that CVI has become a leading cause of visual impairment in children in developed countries,1-3 as well as in lower and middle income nations, making it a growing global health concern. In a national registry that collected data on 2,155 children with visual impairment in the U.S., from birth to age 3, CVI was the most prevalent diagnosis (24%), followed by retinopathy of prematurity (ROP) (16%) and optic nerve hypoplasia (10%). 4
In countries with national healthcare systems that more widely track causes of visual impairment, such as the United Kingdom, CVI accounts for up to 48% of cases of severe childhood visual impairment and blindness.5,6 CVI accounted for 27% of such cases in the Netherlands.7
Children with CVI can have a range of visual deficits and every case is unique. They may have poor visual acuity or limited field of vision. In addition, they may have higher-order visual processing deficits that interfere with attention and recognition. A person with CVI may miss important details. In a crowd, even family faces may be unrecognizable; a favorite toy may be undetectable in a cluttered box. Difficulty coordinating motor movements using visual cues can be challenging for some with CVI.

Michael Jackel. Credit: Bernadette Jackel
As a child, Michael Jackel would frequently fall when he encountered stairs because he couldn’t see anything in his lower visual field. Eventually, he learned that handrails were a cue to be alert for them. At age 30, he uses a cane in unfamiliar environments to detect stairs and manage his lack of depth perception.
CVI’s impact on functional vision may be more evident in certain environments or under certain conditions. For Jackel, noisy rooms interfere with his ability to see things directly in front of him. Other people with CVI have difficulty seeing in unfamiliar or cluttered environments.
What causes CVI and why might its prevalence be increasing?

Magnetic resonance imaging scan shows an adolescent with CVI associated with prematurity. Enlarged ventricles with irregular sulcal patterns (folds) in the occipital pole (a hallmark sign of periventricular leukomalacia, PVL) are apparent (arrow). Credit: Lotfi Merabet
Complications from premature birth are one of the leading causes of CVI. During the second half of pregnancy the brain is rapidly developing, making it particularly vulnerable to certain types of injury such as periventricular leukomalacia (PVL). PVL is associated with damage to the developing neurons and support cells in many parts of the brain, especially in areas responsible for motor function and visual processing. As a result, infants with PVL have a higher likelihood of developing cerebral palsy and CVI.
CVI can also be caused by complications during a full-term pregnancy or childbirth, such as infection and prolonged oxygen deprivation and brain malformations during fetal development. Shaken baby syndrome or any type of traumatic brain injury later in life can disrupt the visual processing centers. Metabolic and genetic disorders have also been linked with CVI.
Advances in neonatal care have dramatically improved survival rates of extremely premature infants (less than 28 weeks gestation). Between 1993 and 2012, the percentage of surviving infants born at 23 weeks’ gestation increased from 52% to 65%.8
Higher survival rates after premature birth may mean that more children are at potential risk for CVI.
At the same time, rates of pediatric vision loss from preventable ocular causes, such as retinopathy of prematurity and congenital cataracts, have declined precipitously in developed countries. As a result, CVI now accounts for a greater percentage of vision impairment among children in the community and also in schools such as Perkins.
Diagnosing CVI
Evidence-based guidelines for CVI diagnosis are lacking. “Diagnosis really depends on the healthcare provider’s level of experience and suspicion that a child is having difficulty seeing because of functional vision deficits due to neurological damage,” said Lotfi Merabet, O.D., Ph.D., MPH, associate professor of ophthalmology at Massachusetts Eye and Ear and Harvard Medical School.
If a child is not meeting age-appropriate visual developmental milestones, such as holding direct eye contact, following a slow-moving object, or reaching for objects, CVI should be considered along with eye problems.
CVI assessment should consider both visual function and functional vision. Visual function measures eye health, visual acuity, contrast sensitivity, visual field, color perception, and eye mobility. Functional vision gauges ability to use vision for daily activities. Many people with CVI have normal visual function but still have problems with functional vision.
Evaluating functional vision should incorporate contextual-based behavioral testing, Merabet said. There are very few tools that provide objective measures of functional vision in individuals with CVI.
Currently, CVI assessment relies primarily on questionnaires and observational tools. One such example is the CVI Range, which uses interviews and trained observation to infer how various visual features, such as color, movement, and visual complexity impact a child’s ability to perceive their visual environment. Other screening tools or history taking tools developed in Europe, such as the CVI Questionnaire and CVI Inventory, also help clinicians understand how functional vision is impacted throughout a child’s day.
Complicating diagnosis is the fact that CVI often coexists with other conditions that may be more evident to the external observer, such as cerebral palsy, autism, and attention deficit hyperactivity disorder. Rehabilitative strategies for these conditions are often visually dependent, a fact that underscores the importance of addressing the underlying CVI.
Not surprisingly, CVI is commonly misdiagnosed. “I can’t tell you how many times I’ve heard parents say that they’ve been told ‘Your child’s eyes look fine. The problem is behavioral, or the child has a learning disability.’ It’s an incredibly frustrating scenario for parents who can’t get the right diagnosis,” said Merabet.
Yet getting a CVI diagnosis can be crucial to qualifying for educational services under Part B of the Individuals with Disabilities Education Act (IDEA), which opens access to educational services and accommodations for children with disabilities, including blindness and low vision.
“CVI in high-functioning children often gets written off as a behavioral problem,” said Linda Lawrence, M.D., an ophthalmologist from Salina, Kansas. Lawrence recalled a “clumsy” fourth grader who was doing poorly in school. “Her CVI had been missed for years in part because she had 20/20 vision. It wasn’t until she was diagnosed that her grades improved. She was given a cane to manage her limited lower field of vision and an individualized education program (IEP) that addressed her visual needs. It was life changing,” said Lawrence, who is a consultant member of the Pediatric Low Vision Rehabilitation Committee for the American Association for Pediatric Ophthalmology and Strabismus.
Similarly, Michael Jackel was denied accommodations because standard vision testing failed to show a problem. According to his mother, Bernadette Jackel, none of Jackel’s teachers were prepared to instruct a child with CVI. “School was a nightmare,” she said. “By seventh grade, Michael was convinced that he was stupid and couldn’t learn.”
Schools often lack the expertise to teach children with CVI, said Amanda Lueck, Ph.D., professor emerita of special education at San Francisco State University. Standard educational and rehabilitative approaches for people with low vision—such as magnifying text or improving contrast—fail to address the brain-based issues of CVI. “We are in the very early days when it comes to figuring out what rehabilitative strategies work in CVI. And what works for one child with CVI, doesn’t necessarily work for another,” she said.
Lacking evidence-based approaches, the best current strategy is to involve a multidisciplinary team with expertise in neurology, occupational and physical therapy, and orientation and mobility training, she said.
Desperate for an environment that could address his needs, Jackel enrolled as a boarding student at Perkins where he stayed until he graduated high school. Perkins made a huge difference in Jackel’s ability to progress academically, according to his mother. His typical class size went from 20 to four students. Classrooms were less cluttered. And lessons accommodated his needs; for example, teachers helped him read by presenting one word at a time.
New research may hold key to successful rehabilitation
With funding from the National Eye Institute (NEI), part of the National Institutes of Health, Merabet is attempting to quantify CVI-related changes to the brain and functional vision deficits, and compare those changes with ones that occur in ocular-based visual impairment, as a step toward gauging which rehabilitative strategies might eventually work best.
Using brain imaging studies, he also hopes to better define CVI neurologically and physiologically.
The work is based on an earlier study with Corinna Bauer, Ph.D., also of Massachusetts Eye and Ear and Harvard Medical School. Together, they used a combination of imaging tests to explore the effect of blindness on the brain. They found that people who lose their vision very early in life due to ocular blindness tend to have reorganized structural and functional connections in their brains, relative to those of sighted individuals. Early blindness caused reductions in the size of visual processing structures. But brain regions involved in other functions, such as hearing and language processing, showed enhanced brain connectivity. As of yet, it is unclear how the brain changes in the setting of CVI. “Studies that provide clues about how the brain functions and adapts could bring evidence-based strategies to CVI rehabilitation,” said Merabet.10
Merabet hopes to find out if people with CVI have similar indications of brain plasticity. “We are comparing brain plasticity in CVI with individuals with ocular based impairment,” he said.
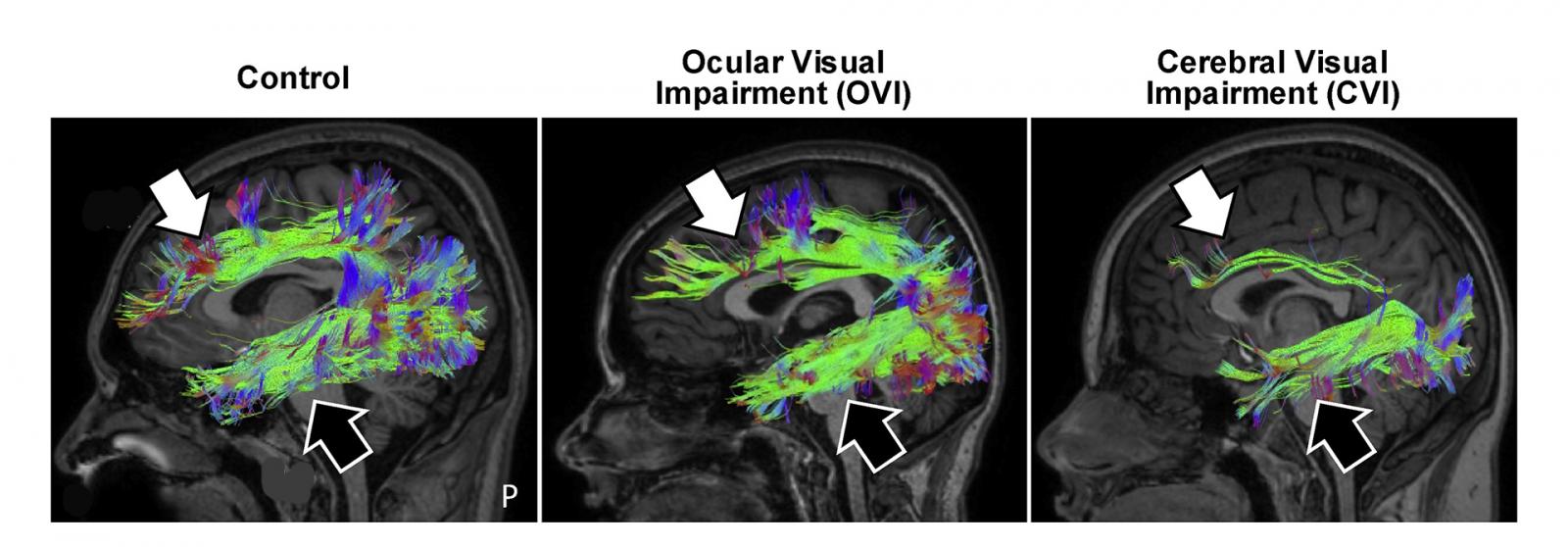
Diffusion based imaging reveals that dorsal (white arrow) and ventral (black) visual processing streams remain intact in people with ocular causes of visual impairment, but are markedly reduced in individuals with CVI (particularly the dorsal stream implicated with spatial processing). 9
Merabet has also developed a virtual reality-based platform to assess CVI’s impact on a person’s functional vision. The system tracks and records a person’s eye movements as they explore and look for a specific target in a simulation of a real-world setting. For example, users are asked to identify a specific toy in a cluttered virtual toy box as various features of the visual scene are changed to make the task more difficult. In an another NEI-funded study, Merabet is validating the system’s usefulness for quantifying functional vision deficits, which will help lay the groundwork for developing adaptive tools and strategies to meet an individual's specific rehabilitative needs.
Other NEI-funded research is aimed at objectively evaluating what people with CVI can and cannot see, especially in situations where a significant intellectual disability interferes with the ability to communicate or read an eye chart.

It can be difficult to quantify functional vision deficits among people with CVI. This heat map shows visual search patterns for a virtual toy box task with yellow representing more time spent looking at an area and blue indicating less time. Note how in CVI the extent of visual area explored increases with greater task demand. Merabet hopes that such virtual reality (VR) based tools will help better assess functional vision impairments in CVI.9
Toward that end, with NEI funding, Glen Prusky, Ph.D., director of the Laboratory for Visual Disease and Therapy at Burke Neurological Institute, White Plains, New York, developed a system that tracks eye movement to gauge how well a child with CVI can see.
His system is based on observation of a reflexive behavior: When our eyes track an object gliding across our field of vision, they move smoothly. Take the object away, and without anything to focus on, our eyes are unable to move smoothly. Building on that idea, Prusky’s system assesses how well a child sees by presenting him or her with a large visual stimulus drifting across a computer screen. An infrared eye tracker plots where the child is looking, and an algorithm determines whether the child’s eye movements are smooth, indicating their fixation on the stimulus. When the child smoothly tracks, they are incentivized to keep trying to focus by being rewarded with a favorite song. The stimulus becomes increasingly difficult to see in order to identify the limit of a child’s functional vision.
“It’s really remarkable to see a child lying in bed not looking at much or tracking. And then you put this screen in front of them and you move stuff and almost like a light bulb you see them become engaged,” Prusky said.
Merabet’s research is funded by NEI grants R21EY030587 and R01EY031300. Prusky’s research is supported by NEI grant R01EY030156.
References:
1 Chang, M. Y. & Borchert, M. S. Advances in the Evaluation and Management of Cortical/Cerebral Visual Impairment in Children. Survey of Ophthalmology, doi:https://doi.org/10.1016/j.survophthal.2020.03.001 (2020).
2 Khan, R. I., O'Keefe, M., Kenny, D. & Nolan, L. Changing pattern of childhood blindness. Ir Med J 100, 458-461 (2007).
3 Kong, L., Fry, M., Al-Samarraie, M., Gilbert, C. & Steinkuller, P. G. An update on progress and the changing epidemiology of causes of childhood blindness worldwide. Journal of American Association for Pediatric Ophthalmology and Strabismus 16, 501-507, doi:https://doi.org/10.1016/j.jaapos.2012.09.004 (2012).
4 Hatton, D. D., Schwietz, E., Boyer, B. & Rychwalski, P. Babies Count: The national registry for children with visual impairments, birth to 3 years. Journal of American Association for Pediatric Ophthalmology and Strabismus 11, 351-355, doi:https://doi.org/10.1016/j.jaapos.2007.01.107 (2007).
5 Rahi, J. S. & Cable, N. Severe visual impairment and blindness in children in the UK. The Lancet 362, 1359-1365, doi:https://doi.org/10.1016/S0140-6736(03)14631-4 (2003).
6 Durnian, J. M. et al. Childhood sight impairment: a 10-year picture. Eye 24, 112-117, doi:10.1038/eye.2009.32 (2010).
7 Boonstra, N. et al. Changes in causes of low vision between 1988 and 2009 in a Dutch population of children. Acta Ophthalmologica 90, 277-286, doi:10.1111/j.1755-3768.2011.02205.x (2012).
8 Stoll, B. J. et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993-2012. JAMA 314, 1039-1051, doi:10.1001/jama.2015.10244 (2015).
9 Bennett, C. R., Bauer, C. M., Bailin, E. S. & Merabet, L. B. Neuroplasticity in cerebral visual impairment (CVI): Assessing functional vision and the neurophysiological correlates of dorsal stream dysfunction. Neuroscience & Biobehavioral Reviews 108, 171-181, doi:https://doi.org/10.1016/j.neubiorev.2019.10.011 (2020).
10 Bauer, C. M. et al. Multimodal MR-imaging reveals large-scale structural and functional connectivity changes in profound early blindness. PLOS ONE 12, e0173064, doi:10.1371/journal.pone.0173064 (2017).
Resources for more information about CVI
CVI information from the National Eye Institute
CVI Now, Perkins School for the Blind
https://www.perkins.org/cvi-now
CVI Now, Q&A with Dr. Lotfi Merabet
https://www.perkins.org/cvi-now/understanding-cvi/cvi-brain-dr-lotfi-merabet
CVI Scotland
Cortical/Cerebral Visual Impairment, Traumatic Brain Injury, and Neurological Vision Loss
(American Foundation for the Blind)
https://www.afb.org/blindness-and-low-vision/eye-conditions/cortical-visual-impairment-traumatic-brain-injury-and
Cortical Visual Impairment (American Association for Pediatric Ophthalmology and Strabismus)
https://aapos.org/browse/glossary/entry?GlossaryKey=b1bcb5d7-98a8-4938-b9fd-bbf73fdeb386
Cortical Visual Impairment: What Is It? (Discovery Eye Foundation)
http://discoveryeye.org/cortical-visual-impairment-what-is-it/