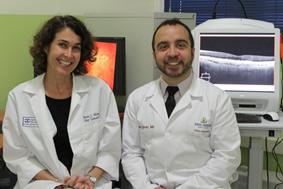
Dr. Rachel Bishop and Dr. Allen Eghrari, from the Johns Hopkins University Wilmer Eye Institute, shown here with the advanced imaging technologies being used for the PREVAIL III study in Monrovia, Liberia.
Following the 2014 Ebola outbreak in West Africa that took the lives of more than 11,200 people in the region, the National Eye Institute, part of the National Institutes of Health, has deployed a team of clinicians and technical experts to Monrovia, Liberia to investigate the effects of Ebola on the eye.
NEI’s investigation is part of a larger study called PREVAIL III (Partnership for Research on Ebola Virus in Liberia) aimed at understanding the long-term health implications of Ebola virus disease (EVD) among people who survived acute infection with the virus. Of the estimated 15,000 survivors in Liberia, Guinea and Sierra Leone, many report a variety of ailments from headaches and tinnitus, to joint and muscle pain, eye fatigue and blurry vision.
While physicians have some understanding about how to manage the infection during the acute phase, their strategies are experimental at this point and much is still unknown about the natural history of Ebola virus, including in the eye and its long-term effects on ocular health and vision, said Rachel Bishop, M.D., M.P.H., chief of the Consult Services Section at NEI and part of the NIH team working in Liberia. Dr. Bishop recently coauthored a viewpoint on Ebola and the Eye published in JAMA Ophthalmology.
Some viruses have been known to linger in the eye after a person has recovered from acute illness and the blood is virus-free. This appears true of Ebola, a fact that Dr. Bishop emphasizes does not put other people at risk of becoming infected because the virus is inside the eye, not on the surface. Nor is there any evidence that live virus is present in survivors’ tears. But transmission associated with the eye could be a potential concern in the future if eye surgery should be needed.
There have been reports of uveitis among Ebola survivors since the 1990s. Uveitis is an inflammatory eye disease that has a variety of causes including infection. Among Ebola survivors, it tends to respond well to corticosteroids, which suppress inflammation.
Based upon those earlier reports, it was anticipated that some people who had survived Ebola during the recent epidemic in West Africa would develop uveitis and that has indeed been the case. However, “there are still many unanswered questions,” Dr. Bishop said. “At this point we don’t know the extent of the effect of Ebola on the eye. We’ve seen changes to nearly every part of the eye among Ebola survivors, including many changes in the retina [the light-sensitive part of the eye]. And some survivors are having vision problems such as difficulty focusing and eye fatigue, the causes of which remain elusive.” Some Ebola survivors show signs of cognitive changes after the infection, which could also contribute to vision difficulties, she said.
PREVAIL III is sponsored by the National Institute of Allergy and Infectious Diseases in partnership with the Liberian Ministry of Health, and will be conducted at several sites in Liberia. The objective is to enroll up to 7,500 people, including 1,500 people who survived Ebola and up to 6,000 of their close contacts to serve as a control group. After a baseline examination and survey, participants will be evaluated every six months for five years.
The goal is to determine the cause of various EVD-related symptoms and how best to treat them. Survivors also are being assessed to see whether they develop immunity that will protect them from future Ebola infection, and to determine the risk of transmitting the virus to close contacts and sexual partners. In addition to the eye, the virus appears to persist in the testes; semen has been shown to carry live virus many months after recovery and clearance of the infection from the blood. The PREVAIL III investigators will be tracking viral counts in semen to understand more about the risk of infection for sexual partners over time.

The PREVAIL eye clinic team assembled includes nurses, technicians, and administrative support staff.
In March 2015, renovations began on an entire floor of the John F. Kennedy Medical Center in the Liberian capital, Monrovia, to establish a patient clinic for PREVAIL III.
Along with Allen Eghrari, M.D., from the Johns Hopkins University Wilmer Eye Institute, the NEI team oversaw the design of an eye clinic, which is outfitted with state-of-the-art diagnostic equipment and is in many ways as advanced as the eye clinic in the NIH’s Clinical Center.
Access to such advanced diagnostic equipment is important for visualizing and documenting changes in the eye, said Denise Cunningham, chief of the Imaging Services Section at NEI, who visited the Liberian clinic for two weeks this year to train the staff how to use the technology. Now when abnormalities are seen on a slit lamp exam, the patients can be referred for a far more detailed evaluation using optical coherence tomography (OCT). With OCT, cross sections and color images can be taken so the damage can be outlined visually and any changes over time can be monitored.
NEI’s Guy Foster, chief of the Clinical Services Section, spent two weeks at the Liberian clinic getting the diagnostic equipment up and running. Frequent power outages throughout the day presented a key challenge. In addition to disrupting eye exams, the unreliable power supply posed a major potential hazard to the diagnostic equipment, which is sensitive and could have easily been damaged from power surges. Foster’s solution was to step down the voltage and install a power conditioner, which helps maintain a steady flow of electricity. Now the clinic is running successfully without power interruption.
The NEI team plans to travel back to Liberia for periodic visits over the course of the study, and is assisted by a permanent local eye care team they trained to conduct vision screening and other tests. The team includes nurses, technicians, and administrative support staff. They are also working with Liberian ophthalmology partners who are helping to provide follow-up eye care in the clinic for study participants needing treatment.
“Despite the tragedy that the Liberians have endured, you get a sense of positive energy and liveliness – so it’s actually a happy place to work. It’s a true collaboration,” Dr. Bishop said.
Cunningham agreed. “The Liberian people have endured so many hardships. The Ebola epidemic was one more. And yet they have this resilience.” The Liberians working on the PREVAIL team are “so eager to learn and contribute to the success of the study. They’ve been a great team to work with.”
They’re also extremely grateful, said Foster, remembering an exchange he had with an ophthalmologist working at an outlying clinic. “This man was used to sticking a flashlight on top of the slit lamp to examine his patients’ eyes. No LED bulbs. No electricity. The ocean air corrodes the equipment so nothing really functions well, and yet they are still trying to see patients. I showed him what we are doing in the clinic and he hugged me. He said ‘Now I can treat patients. I was about to give up.’
- By Kathryn DeMott
Reference:
Jampol LM et al, “Ebola and the Eye,” published online July 23, 2015 doi:10.1001/jamaophthalmol.2015.2400